What is Glaucoma?
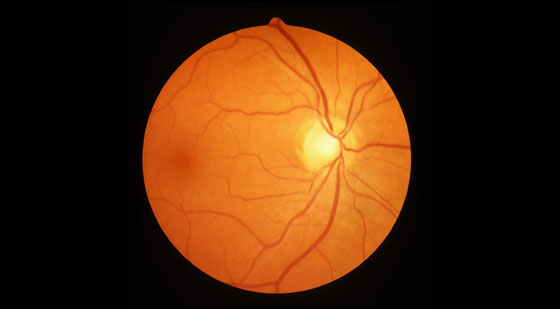
Glaucoma is the name given to a group of eye diseases in which the optic nerve at the back of the eye is slowly destroyed. In most people this damage is due to an increased pressure inside the eye – a result of blockage of the circulation of aqueous, or its drainage. In other patients the damage may be caused by poor blood supply to the vital optic nerve fibres, a weakness in the structure of the nerve, and/or a problem in the health of the nerve fibres themselves.
Damage to the optic nerve can eventually cause loss of peripheral vision. Advanced stages of this condition could result in tunnel vision.
Over 300,000 Australians have glaucoma. While it is more common in older patients, it can occur at any age.
Types of Glaucoma
POAG (Primary Open Angle Glaucoma) – This is the most common and chronic type of glaucoma. It is usually painless and patients with a eye pressure of above 20mmHg will need to be monitored or treated.
NTG (Normal Tension Glaucoma) – Patients will present with what appears to be a ” normal eye pressure” normally between 10 and 21. If there appears to be damage to the optic nerve the patient will be monitored or treated.
NAG (Narrow Angle Glaucoma) – People with this type of glaucoma have an anatomically narrow drainage system which means aqueous humor is slower to drain out. This can lead to consistently higher eye pressure which may cause damage to the optic nerve. Additionally people with is condition are at risk of AACG.
AACG (Acute Angle Closure Glaucoma) – This is an acute condition where the iris (coloured front part of the eye) blocks the drainage system in the front of the eye. The aqueous humor cannot flow as usual – causing a pressure spike which in turn causes blurred vision, a painful eye, nausea and vomiting.
Secondary Glaucoma – Glaucoma caused secondary to another condition – e.g trauma to the eye, cataracts, strokes in the eye, steroid use and inflammatory eye conditions.
Congenital Glaucoma – when a child is born with abnormal drainage system. Child may display excessive watery eyes and light sensitivity as well as the appearance of enlarged cloudy eyes.
What are the risk factors for Glaucoma?
Anyone can be diagnosed with this condition however people will have higher risk of glaucoma if they have the following:
- Family history.
- Trauma to the eye.
- Myopia (Short sightedness).
- Hypermetropia (Long sightedness).
- Corticosteroid use in the past or present.
- Smoke cigarettes.
What are the symptoms of Glaucoma?
Certain types of glaucoma can result in high pressure within the eye. This can lead to following:
- Sore painful red eye.
- Blurred vision.
- Haloes around lights.
- Pressure sensation behind the eye.
- Headaches at night.
- Sudden loss of vision.
- Advance stage of this disease can result in tunnel vision which can lead to trouble navigating around.
The best way to detect this condition is to see your local optometrist for an eye check-up by the age of 40. It should be sooner from the age of 35 years if you have any of the associated risk factors.
People of the African or the Asian population should have an eye examination by the age of 40 years and the Caucasian population by 50 years of age.

How is Glaucoma diagnosed?
Initially a series of tests and baseline measurements of the eye will need to be performed.
Patient History: Helps determine individual risks
Family History: Identifies if anyone in the family has Glaucoma
Corneal Pachymetry: Measures the thickness of the cornea (Front of the eye).
Applanation Tonometry: Measures the eye pressure.
Gonioscopy: Assesses the drainage network inside the front of the eye for potential narrowing and blockage.
OCT Scans (Optical Coherence Topography): A non-invasive scan of the optic nerve and the nerve fibre bundle layers.
Automated Visual Field Testing: It is a subjective test to map the peripheral vision to assess glaucoma damage.
Treatment / Management
Management: After diagnosis, patients are usually seen every 6-12 months to monitor their condition. Usually Applanation tonometry, OCT scan and the automated visual field are performed again.
Types of treatment:
Eye Drops: Glaucoma is primarily managed by medicated eye drops which are instilled once or several times daily indefinitely. Management of glaucoma may require more than one type of drop ( e.g a combination of two or more drops).
SLT (Selective Laser Trabeculoplasty) laser: Laser is fired into the drainage system at the front part of the eye, which stimulates tissue to allow better drainage outflow. It is a low strength laser which is less damaging to the structures of the eye and can be repeated if necessary.
PI (Peripheral Iridotomy) YAG laser: This type of laser is a higher strength laser and is used as a preventative treatment when a patient is found to have a narrow drainage system and have a higher chance of acute angle closure glaucoma. It is also used when a patient presents with acute angle closure glaucoma. It opens a channel for aqueous drainage.
Surgery: Surgery is usually performed when eye drops and laser cannot adequately lower the eye pressure. This would involve creating an alternative drainage system to allow the aqueous humour to flow out of the eye. As with any type of surgery there is always risk of infection, however there is also a risk that the eye pressure does not fall.

