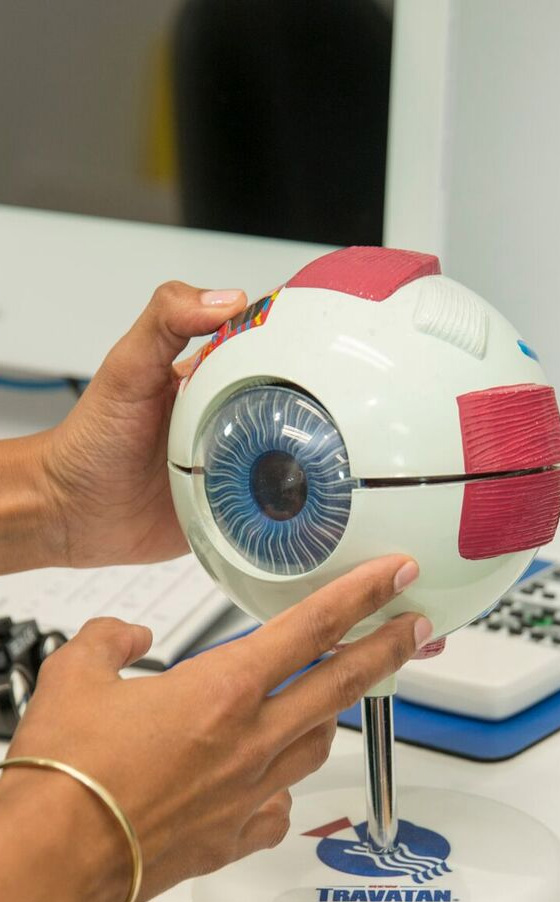
The cornea is the transparent, dome shaped window at the front of each eye. It plays an important role in focusing your vision. It needs to be clear and normally shaped for you to see properly.
Although the cornea is clear, it actually contains five layers. Knowing about these layers can help you to understand corneal diseases. The layers are:
- Epithelium
This is the very outer later. The corneal epithelium protects the eye from foreign material (dust, water, bacteria) and absorbs oxygen and nutrients from tears. The epithelial cells are anchored onto a membrane called the basement membrane.
The epithelium contains thousands of tiny nerve endings. This is why a tiny eyelash or speck of dust can cause so much irritation.
- Bowman’s membrane
The next layer of the epithelium consists of collagen fibres. If injured, these can scar and potentially cause vision loss.
- Stroma
Behind Bowman’s layer is the stroma. This is the thickest layer of the cornea. It mainly consists of water and collagen. The collagen fibres provide strength, elasticity and shape.
- Descemet’s membrane
The next layer of the cornea is a thin but strong film of tissue. It is also made of collagen fibres but they are different from the stromal collagen fibres. Descemet’s membrane protects against infection and injuries. It heals easily and rapidly after injury.
- Endothelium
The endothelium is the thin, innermost layer of the cornea. It pumps out the fluid that leaks from inside the eye into the stroma. Without this function, the stroma would swell and become opaque.
This layer doesn’t heal well after injury or disease.
There are many conditions and disease that affect the cornea.
What common conditions affect the cornea?
Allergies
Pollens tend to be the most common eye allergen.
Symptoms include:
- Redness
- Itching, burning or stinging
- Tearing/watery eyes
Antihistamines often work well to reduce these symptoms.
Dry eye
Dry eye occurs when the eye doesn’t produce enough (or high enough quality) tears to keep the cornea lubricated.
Injuries
Minor corneal injuries or scratches are common but usually heal up quickly. Deeper injuries may cause scarring, which can affect your vision.
Symptoms of a deeper corneal injury include:
- Eye pain
- Sensitivity to light
- Blurry vision
- Redness or inflammation in the eye
- Headache
If you have any of these symptoms, see an eye care specialist.
Keratitis
Keratitis means inflammation of the cornea. The most common cause of keratitis is infection, which may be caused by bacteria, viruses, fungi or parasites. Non-infectious causes include minor injury or from wearing contact lenses for too long.
Minor infections can be treated with antibiotics eye drops. More severe infections may require more intensive antibiotics and anti-inflammatories.
What diseases can affect the cornea?
Herpes zoster (Shingles)
Shingles is a reactivation of the virus that causes chickenpox. Once you’ve had chickenpox, the virus can lay dormant in your nerve cells. It can then ‘wake up’ later on in life and travel through nerve fibres, including nerve fibres to the cornea. This can lead to pain, inflammation and scarring.
Corneal problems can occur months after signs of shingles have cleared the rest of the body. If you experience shingles in your eye, nose or on your face, have your eyes checked several months after shingles has resolved.
Ocular herpes
You can have a recurrent herpes infection of the eye. Either of the types of herpes simplex virus that cause cold sore or genital herpes may be involved.
Ocular herpes can produce sores on the eyelid or the surface of the cornea. It can spread into the deeper levels of the cornea and cause a more severe infection called stromal keratitis.
Iridocorneal endothelial syndrome
Iridocorneal endothelial syndrome (ICE) is caused by the movement of endothelial cells from the cornea to the iris. This transfer of cells creates three main features:
- Visible changes in the iris
- Swelling of the cornea (without the endothelial cells pumping fluid out of the cornea, it swells)
- Glaucoma – the migrated cells block fluid outflow channels leading to increased fluid (and therefore pressure) inside the eye.
There is no treatment to stop the progression of ICE. But the glaucoma is treatable and if the cornea becomes so swollen that vision is impaired, a corneal transplant may be performed.

Pterygium
A pterygium is a pinkish, triangular tissue growth on the cornea.
Stevens-Johnson Syndrome
Stevens-Johnson Syndrome (SJS), or erythema multiforme major, is a disorder of the skin that also affects the eyes. The most common cause of SJS is an allergic reaction to a drug or medication. It is also associated with viral infections.
Symptoms of SJS include:
- Flu-like symptoms
- A painful rash of blisters on the skin and the mucous membranes of the mouth, throat, genitals
- Conjunctivitis
- Corneal blisters, erosions and even corneal holes
Treatments for the eye symptoms include artificial tears or lubricating eye drops, antibiotics and corticosteroids.
Corneal dystrophies
Corneal dystrophies are a group of disease where a build-up of material clouds the cornea. They can affect people in different ways.
Some cause:
- No symptoms and are only discovered during a routine eye exam
- Severe vision impairment
- Repeated episodes of pain without leading to permanent vision loss
Some of the most common corneal dystrophies include:
Keratoconus
Keratoconus is a progressive thinning of the cornea.
Fuchs’ dystrophy
Fuchs’ dystrophy is a slowly progressing disease that worsens vision over many years. Most people with Fuchs’ dystrophy won’t notice vision problems until they reach their 50s or 60s.
It is caused by a gradual dying off of corneal endothelial cells. Without endothelial cells to pump out the fluid that leaks from the inside of the eye into the cornea, it swells and thickens.
As the disease progresses, Fuchs’ dystrophy symptoms usually affect both eyes and include:
- Glare, which affects vision in low light
- Blurred vision that occurs in the morning after waking and gradually improves during the day
- Distorted vision, sensitivity to light, difficulty seeing at night and seeing halos around light at night
- Painful, tiny blisters on the surface of the cornea
- A cloudy or hazy looking cornea
The first step in treating Fuchs’ dystrophy is to reduce the swelling with drops, ointments or soft contact lenses. If you have a severe disease, your eye specialist may suggest a corneal transplant.
Lattice dystrophy
Lattice dystrophy gets its name from a characteristic lattice-like pattern of deposits in the stroma of the cornea. The deposits are made of amyloid, which is an abnormal protein fibre. As more amyloid is deposited, the stroma becomes opaque and vision is impaired.
The deposits can also accumulate under the corneal epithelium. Here they can erode the epithelium and alter the cornea’s normal curvature. This creates temporary vision problems and severe pain due to exposure of the nerves within the cornea. The erosions usually heal within days, although you may have some pain for the 6–8 weeks.
Eye specialists may prescribe eye drops and ointments to ease the pain caused by the friction of the eyelid against the cornea. In some cases, an eye patch may be used to immobilise the eyelid.
Lattice dystrophy typically begins in childhood. By age 40, some people have so much scarring under the epithelium that the most effective treatment is a corneal transplant.
Although the early results of corneal transplantation are typically good, lattice dystrophy may appear again later.
MapDot-Fingerprint dystrophy
Map-Dot-Fingerprint dystrophy occurs when the basement membrane develops abnormally and forms folds. The folds create grey shapes that look like continents on a map. There also may be clusters of opaque dots underneath or close to the map like patches. Occasionally, the folds form concentric lines in the central cornea that resemble small fingerprints.
Symptoms include:
- Blurred vision
- Pain in the morning that lessens during the day
- Sensitivity to light
- Watery eyes
- A feeling that there’s something in the eye
Typically, symptoms flare up now and then over the course of several years and then go away, without vision loss.
Some people with Map-Dot-Fingerprint dystrophy develop recurring epithelial erosions. These alter the cornea’s normal curvature and cause blurred vision. They may also expose the nerve endings within the cornea, resulting in moderate to severe pain that lasts several days.
An eye specialist may prescribe lubricating eye drops or ointments to manage the pain. If drops or ointments don’t relieve the pain, there are surgical procedures that may help. These include:
- Anterior corneal puncture to help the cells adhere better to the tissue
- Corneal scraping to remove eroded areas of the cornea and allow healthy tissue to regrow
- Laser surgery to remove surface irregularities on the cornea
