What is Diabetic Retinopathy (DR)?
Diabetic retinopathy is a serious diabetic eye disease. It is the main cause of preventable blindness in the working Australian population.
The tiny blood vessels located in light sensitive tissue in the back of the eye known as the retina are damaged by diabetes. Diabetic retinopathy can cause blood vessels in the retina to leak fluid or haemorrhage (bleed) – distorting vision. If this condition is not monitored and managed, it may lead to blindness.
Types of Diabetic Retinopathy
Non-proliferative diabetic retinopathy (NPDR) – This is also known as background diabetic retinopathy (BDR). There are three stages which are termed; mild, moderate and severe.
Damage occurs within the layers of the light sensitive area in the back of the eye known as the retina.
Some signs seen are:
- Microaneurysms (abnormal swelling of the tiny blood vessels).
- Blocked blood vessels causing poor blood supply to nourish the retina.
- Growth of abnormally weak blood vessels (due to poor blood supply).
- Hard exudates (blood vessels leak out fatty deposits and cholesterol into the retina).
- Diabetic macular oedema (DME, swelling of the macula which is the area in the retina used for our central vision).
- Macular Ischaemia (loss of blood supply to the central vision of the retina).
Proliferative diabetic retinopathy (PDR) – This is the fourth and most advance stage of diabetic retinopathy. It will have signs of NPDR.
At this stage, this condition worsens and there is poor blood supply to the retina. Abnormal, weak blood vessels grow to try and nourish the retina. These vessels can bleed without warning into the vitreous gel (Jelly like substance found in the eye back part of the eye).
The abnormal vessels can cause scarring and tension. This can cause the retina to wrinkle or retinal detachment.
What are the symptoms of Diabetic Retinopathy?
The early stages of diabetic retinopathy usually have no symptoms. The disease often progresses unnoticed until it affects vision. Bleeding from abnormal retinal blood vessels can cause the appearance of “floating” spots or distortion. Not seeking prompt treatment can increase the risk of permanent vision loss. As the condition progresses and advances the following symptoms may occur:
- Straight lines appear distorted.
- Missing, or jumping letter/words when reading.
- Blurred vision.
- Dark, blurry, grey spots appear in the central vision.
- Flashes of light.
- Sudden loss of vision.
Patient should see their Ophthalmologist for a routine check up to prevent symptoms presenting.
Risk Factors for Diabetic Retinopathy (DR)?
People with all types of diabetes (type 1, type 2, and gestational) are at risk for diabetic retinopathy. Risk increases the longer a person has diabetes. Women who develop or have diabetes during pregnancy may have rapid onset or worsening of diabetic retinopathy.
Risk Factors include:
- Uncontrolled blood sugar levels.
- Uncontrolled high blood pressure.
- Poorly controlled lipid levels.
- Poor diet.
Women who were diagnosed with gestational diabetes or polycystic ovary syndrome are at increased risk of developing type 2 diabetes and may develop DR later in life.
Genetics can affect the onset, severity and speed of DR.
Indigenous Australians and Torres Strait Islander Australians are more likely to develop diabetes compared to the rest of the Australian population. This increases their chance of DR
Other groups at high risk are people of Middle Eastern and Asian populations and Pacific Islanders.
How is Diabetic Retinopathy diagnosed?
Diabetic retinopathy is diagnosed by the ophthalmologist through a comprehensive eye examination using a special microscope called a slit lamp.
Pupil dilation will be required to allow for a thorough evaluation of the macula, retina and optic nerve.
Testing that may occur includes:
- Visual acuity testing – This eye chart test measures a person’s ability to see at various distances.
- Tonometry – This test measures the pressure inside the eye.
- Pupil dilation – Drops placed on the eye’s surface dilate (widen) the pupil, allowing a physician to examine the retina and optic nerve.
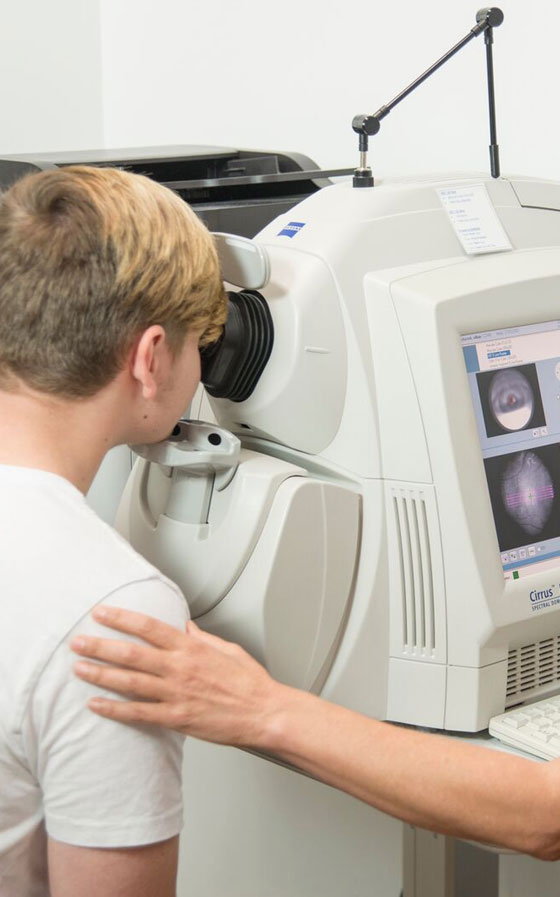
- Optical coherence tomography (OCT) – This technique is similar to ultrasound but uses light waves instead of sound waves to capture images of the tissues inside the body. OCT provides detailed images of tissues that can be penetrated by light, such as the eye.
A comprehensive dilated eye exam allows the doctor to check the retina for:
- Changes to blood vessels
- Leaking blood vessels or warning signs of leaky blood vessels, such as fatty deposits
- Swelling of the macula (DME)
- Changes in the lens
- Damage to nerve tissue
If DME or severe diabetic retinopathy is suspected, a fluorescein angiogram may be used to look for damaged or leaky blood vessels. In this test, a fluorescent dye is injected into the bloodstream, often into an arm vein. Pictures of the retinal blood vessels are taken as the dye reaches the eye.

Management / Treatment
Diabetic retinopathy requires regular monitoring by the ophthalmologist. Appointments will depend on the treatment needed.
Regular monitoring and control of blood sugar levels are important as well eating a balanced diet and regular exercise. Lifestyle changes such as; reducing alcohol consumption and to stop smoking.
The ophthalmologist will work with your family doctor, dietitian and endocrinologist to manage uncontrolled blood sugar, blood pressure and blood cholesterol levels.
More than one of the following treatments may be needed to help control diabetic retinopathy.
1. Laser
There are two types of laser treatments. There is the focal laser and the pan-retinal photocoagulation (PRP) laser. Usually more than one PRP laser treatment is required.
Focal laser: Used to seal the leaking retinal blood vessels causing diabetic macular oedema (DME) and to also shrink the abnormal retinal vessels.
PRP laser: Used to treat proliferative diabetic retinopathy (PDR). Laser is applied into the peripheral retina to shrink blood vessels. It also stops the stimulation of abnormal blood vessel growth.
2. Intravitreal Injections
Currently intravitreal injections (Lucentis or Eylea) are the primary form of treatment for diabetic macula oedema (DME). These are anti – VEGF (Vascular Endothelial Growth Factor) drugs. VEGF are proteins within the eye that trigger the growth of abnormal vessels and fluid accumulation within the retinal layers.
Initially three courses of injections are given, normally four weeks apart.
The injection is administered through the Sclera (white part of the eye) and the patient will have plenty of anaesthetic before the injection.
The primary aims of these drugs are to dry out the fluid in the retina and gain visual improvement.
Lucentis (Ranibizumab): Is a TGA approved drug to treat ARMD (Age related macular degeneration). Recently it has been approved to treat diabetic macular oedema and cystoid macular oedema due to retinal vein occlusion.
Eylea (Aflibercept): Is a TGA approved drug to treat ARMD. Recently it has been approved to treat diabetic macular oedema and cystoid macular oedema due to retinal vein occlusion.
What are the risks/side effects of Intravitreal injection?
A patient may experience some irritation and grittiness following the injection. The eye may water but symptoms usually settle down the next day. The antiseptic (betadine) used to prepare the eye for the procedure may be the cause of this sensation.
The ophthalmologist may prescribe their patients antibiotic eye drops or lubricants after the injection.
As with any minor surgery procedure there is a small risk of complication such as infection of the eye. Usually this can be treated with medicated drops and injections.
Surgery
Vitrectomy: This procedure is used to treat severe bleeding into the vitreous (jelly at the back of the eye), and is performed under local or general anaesthesia. Ports (temporary water-tight openings) are placed in the eye to allow the surgeon to insert and remove instruments, such as a tiny light or a small vacuum called a vitrector. The vitreous gel is replaced with either salt solution, gas (avoid air travel for two months) or silicone oil (a second surgery may be needed to remove the silicon oil at a later date). The same instruments used during vitrectomy may also be used to remove scar tissue or to repair a detached retina.
With surgery there is always risk of infection as well as failure to prevent further abnormal vessels bleeding.
